Diabetes is a chronic condition characterized by high blood sugar levels, which can lead to various complications affecting different parts of the body. One such complication is diabetic foot blister, which occurs due to a combination of factors, including neuropathy, poor circulation, and susceptibility to infections.
What is a Diabetic Foot Blister?
Diabetic foot blisters are a common complication of diabetes, often caused by various factors related to the condition. Understanding the causes, appearance, symptoms, prevention methods, treatment options, and potential complications of diabetic foot blisters is crucial for effectively managing this condition and preventing further complications.

Causes of Diabetic Foot Blisters
High Blood Sugar Levels
High levels of glucose in the blood can damage nerves and blood vessels, increasing the risk of developing blisters on the feet.
Neuropathy
Diabetic neuropathy, a type of nerve damage common in diabetes, can result in decreased sensation in the feet, making it more difficult to detect and prevent blisters.
Poor Circulation
Diabetes can also impair blood circulation, leading to delayed wound healing and making individuals more prone to developing blisters and other foot problems.
Infection
Individuals with diabetes are at a higher risk of developing infections due to compromised immune function, which can contribute to the formation of blisters on the feet.
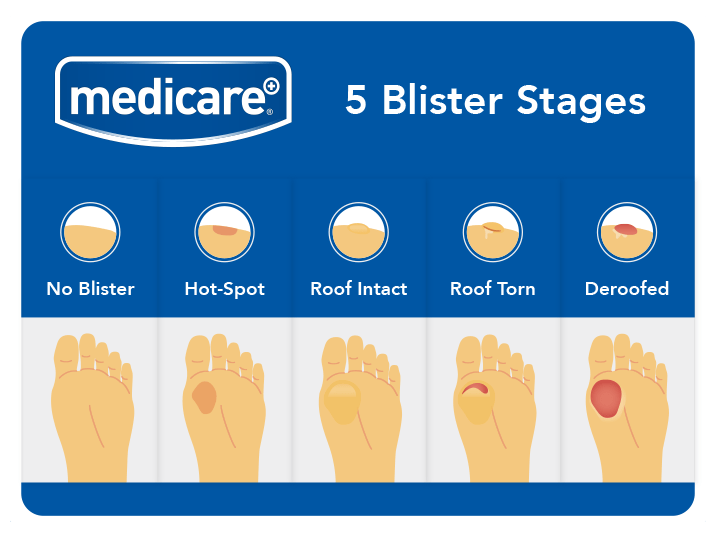
Appearance of Diabetic Blisters
Diabetic foot blisters typically appear as fluid-filled sacs on the skin, ranging in size from small to large. They may be clear or filled with blood and can develop anywhere on the foot, including the toes, heels, and soles.
Symptoms of Diabetic Blisters
Pain
Blisters caused by diabetes may be painful, especially if they become infected or irritated.
Redness or Inflammation
Observe redness or inflammation surrounding the blister, indicative of the body’s response to the affected area.
Itching
Some individuals may experience itching or tingling sensations around the blistered area.

Burning Sensation
In certain cases, diabetic blisters can cause a burning sensation, particularly when pressure is applied to the affected area.
Difficulty Walking
Encounter difficulty walking or putting pressure on the affected foot due to discomfort and sensitivity.
Prevention of Diabetic Foot Blisters
Preventing diabetic foot blisters involves proactive foot care and lifestyle modifications to minimize the risk of complications. Key preventive measures include:
Proper Foot Care
Regularly inspecting the feet for any signs of blisters, cuts, or sores, and keeping the feet clean and dry.
Wearing Appropriate Footwear
Choosing shoes that fit well, provide adequate support, and minimize friction can help prevent blisters and other foot problems.
Avoid Barefoot Walking
Refrain from walking barefoot, especially in environments where injuries are more likely to occur, to protect the feet from potential damage.
Managing Blood Sugar Levels
Maintaining optimal blood sugar control through medication, diet, and exercise can reduce the risk of diabetic complications, including foot blisters.
Draining a Blister
If a blister does develop, it’s essential to drain it safely to prevent infection and promote healing. Here’s how:

- Wash your hands thoroughly with soap and water.
- Clean the blister and surrounding area with an antiseptic solution.
- Use a sterile needle to puncture the blister near its edge.
- Gently press the fluid out of the blister, taking care not to remove the skin covering the blister.
- Apply an antibiotic ointment to the drained blister and cover it with a sterile bandage.
Self-Care Measures for Diabetic Blisters
In addition to draining the blister, taking the following self-care measures can help promote healing and prevent complications:
Keeping the Blister Clean
Regularly washing the blister with mild soap and water and keeping it dry can prevent infection.
Change Bandages Regularly
Regularly change bandages, especially if they become wet or soiled, to maintain a clean environment and prevent further irritation.
Applying Antibiotic Ointment
Applying a thin layer of antibiotic ointment to the blister can help prevent infection and promote healing.
Elevate the Affected Foot
Elevate the affected foot to reduce swelling, alleviate pressure, and improve circulation, aiding in the healing process.
Protecting the Blister
Covering the blister with a sterile bandage or dressing can protect it from further irritation and friction.
Avoid Direct Adhesive Tape Application
Refrain from applying adhesive tapes directly to the blister, as they can exacerbate irritation and hinder healing.
Monitor for Signs of Infection
Regularly monitor the blister for any signs of infection, such as increased redness, swelling, or pus, and seek medical attention if necessary.
Medical Treatments for Diabetic Foot Blisters
In some cases, medical intervention may be necessary to treat diabetic foot blisters, especially if complications arise. Treatment options may include:
Antibiotics
If the blister becomes infected, oral or topical antibiotics may be prescribed to treat the infection.
Debridement
In severe cases, debridement (removal of dead or infected tissue) may be necessary to facilitate healing.
Surgical Intervention
In rare instances, surgical procedures may be required to address complications such as ulceration or gangrene.
Potential Complications
Untreated diabetic foot blisters can lead to various complications, including:
- Infection: Blisters that become infected can spread and lead to more serious infections.
- Ulceration: Untreated blisters may develop into ulcers, which can be difficult to heal and may require extensive treatment.
- Gangrene: In severe cases, inadequate blood flow to the affected area can lead to tissue death (gangrene), necessitating amputation in extreme cases.
When to See Your Doctor
It’s essential to seek medical attention if you experience any of the following symptoms:
- Signs of infection, such as increased pain, redness, swelling, or pus discharge
- Persistent or worsening foot blisters
- Development of ulcers or open sores
- Changes in skin color or temperature
Prompt medical treatment can help prevent complications and promote healing.
In conclusion, diabetic foot blister is a common complication of diabetes that requires careful management and preventive measures to avoid complications. By understanding the causes, symptoms, prevention strategies, and treatment options for diabetic blisters, individuals can take proactive steps to maintain foot health and overall well-being.